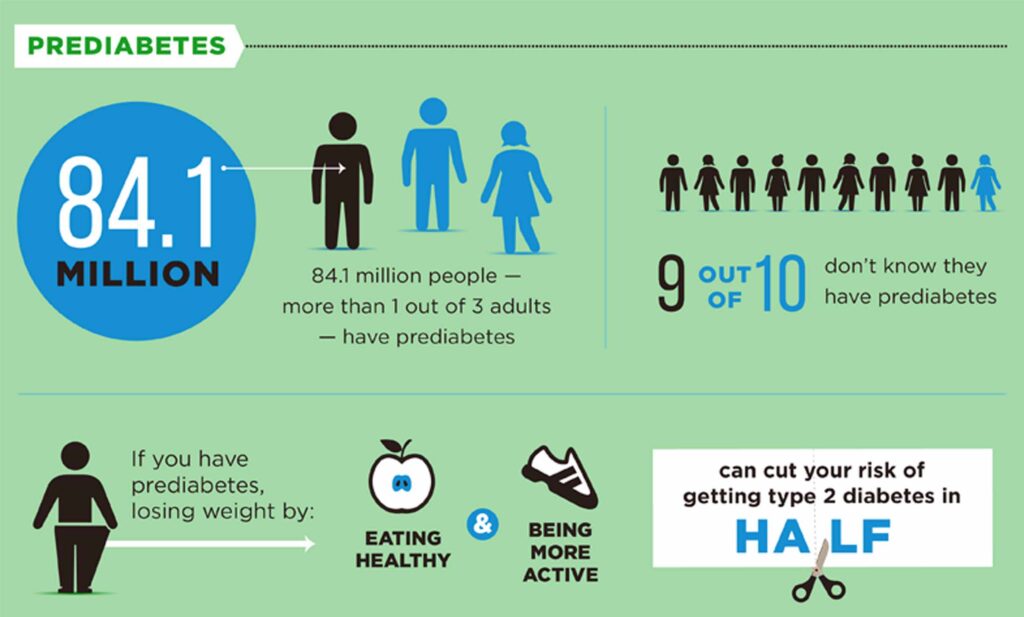
Prediabetes is a condition where blood sugar levels are higher than normal but not high enough to be classified as type 2 diabetes. It indicates an increased risk of developing diabetes and cardiovascular disease.
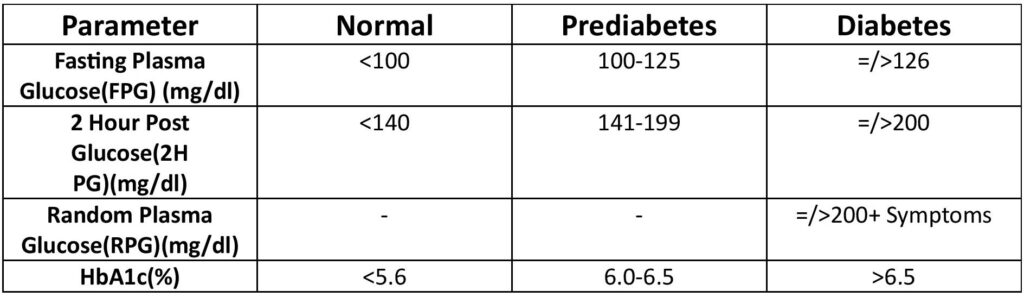
Key indicators of prediabetes include:
- Fasting blood sugar between 100–125 mg/dL (5.6–6.9 mmol/L)
- HbA1c (glycated hemoglobin) levels between 5.7% and 6.4%
- Oral glucose tolerance test (OGTT) results showing blood sugar between 140–199 mg/dL after 2 hours
Lifestyle changes like diet, exercise, and weight management can help prevent the progression from prediabetes to diabetes.
The use of Metformin and SGLT2 inhibitors in prediabetes is an evolving area of research and clinical practice. While both classes of drugs are commonly used in managing type 2 diabetes, their roles in prediabetes are under investigation, particularly for preventing progression to overt diabetes.
Metformin in Prediabetes:
- Metformin is well-established for diabetes prevention, particularly in individuals with high risk of progression to type 2 diabetes. This is based on studies like the Diabetes Prevention Program (DPP), which showed that Metformin reduced the risk of developing diabetes by 31% in people with prediabetes.
- It is especially beneficial in younger individuals with higher BMI and history of gestational diabetes.
- Mechanism: Metformin works by improving insulin sensitivity, reducing hepatic glucose production, and increasing peripheral glucose uptake.
Guidelines:
- The American Diabetes Association (ADA) considers Metformin as a potential pharmacologic option in prediabetes, especially when lifestyle interventions are insufficient or for high-risk patients.
SGLT2 Inhibitors in Prediabetes:
- SGLT2 inhibitors (e.g., empagliflozin, dapagliflozin) are newer agents that work by promoting urinary excretion of glucose, thus lowering blood glucose levels independent of insulin action.
- Their role in prediabetes is less well-defined compared to Metformin, but some studies suggest they could help delay or prevent progression to diabetes by lowering blood sugar, improving glycemic control, and potentially reducing body weight and blood pressure.
Research Insights:
- There is limited data on using SGLT2 inhibitors specifically for prediabetes, but ongoing trials are exploring their effectiveness for diabetes prevention.
- These drugs have additional cardiovascular and renal protective benefits, which may be advantageous in individuals with prediabetes who are at increased risk for heart disease or chronic kidney disease.
Key Considerations:
- Side effects: Metformin is generally well-tolerated, though some individuals may experience gastrointestinal issues. SGLT2 inhibitors can increase the risk of genital infections and dehydration.
- Cost and access: Metformin is inexpensive and widely available, whereas SGLT2 inhibitors tend to be more costly.
- Lifestyle modification remains the cornerstone of prediabetes management, with pharmacologic interventions as an adjunct in high-risk cases.
In conclusion, while Metformin has an established role in the management of prediabetes, the use of SGLT2 inhibitors is still investigational but holds promise for high-risk individuals, particularly those with cardiovascular or renal comorbidities.