Monitoring complications in diabetes involves regular assessments to detect and manage both microvascular and macrovascular complications. This proactive approach can improve outcomes and prevent irreversible damage. Below is an outline for comprehensive monitoring:
Microvascular Complications
1. Diabetic Retinopathy
Screening:
Annual dilated fundus examination by an ophthalmologist.
Fundus photography or optical coherence tomography (OCT) for more detailed imaging.
Signs to Monitor:
Microaneurysms, retinal hemorrhages, or macular edema.
Management:
Optimize blood glucose and blood pressure.
Laser therapy or anti-VEGF injections for advanced cases.
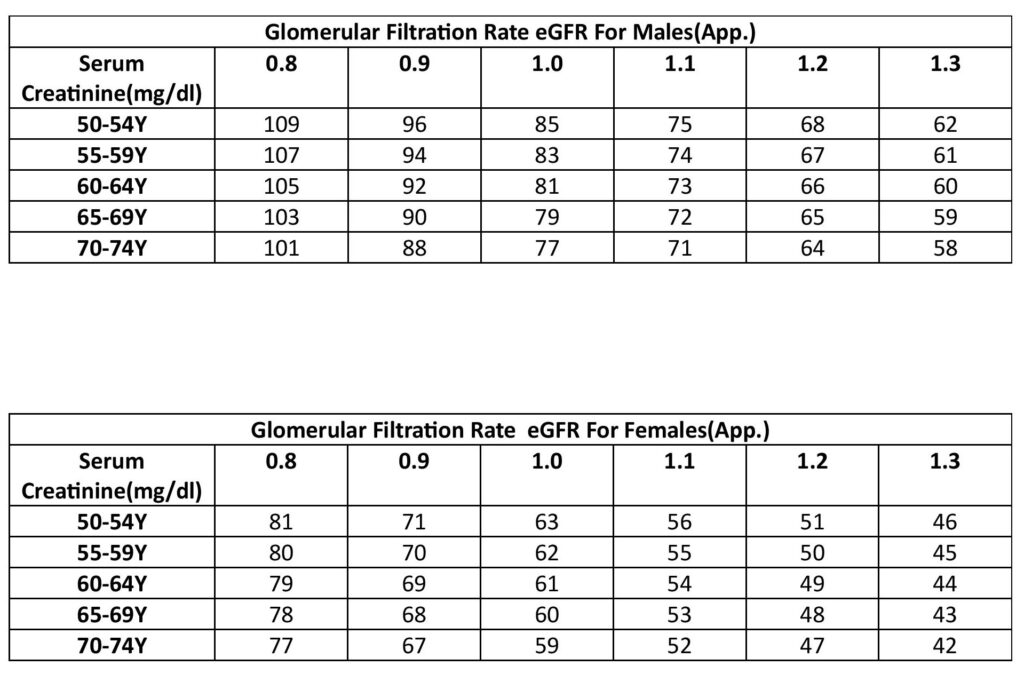
2. Diabetic Nephropathy
Screening:
Annual urine albumin-to-creatinine ratio (UACR).
Serum creatinine and estimated glomerular filtration rate (eGFR).
Signs to Monitor:
Albuminuria, declining eGFR, and hypertension.
Management:
Use of ACE inhibitors or ARBs.
Dietary protein moderation in advanced stages.
3. Diabetic Neuropathy
Screening:
Annual comprehensive foot examination (10-g monofilament, vibration sense, ankle reflexes).
Detailed neurological assessment for autonomic neuropathy symptoms.
Signs to Monitor:
Loss of sensation, tingling, or pain in extremities.
Autonomic symptoms (gastroparesis, orthostatic hypotension).
Management:
Glycemic control, pain management with gabapentinoids or antidepressants.
Education on foot care.
Macrovascular Complications
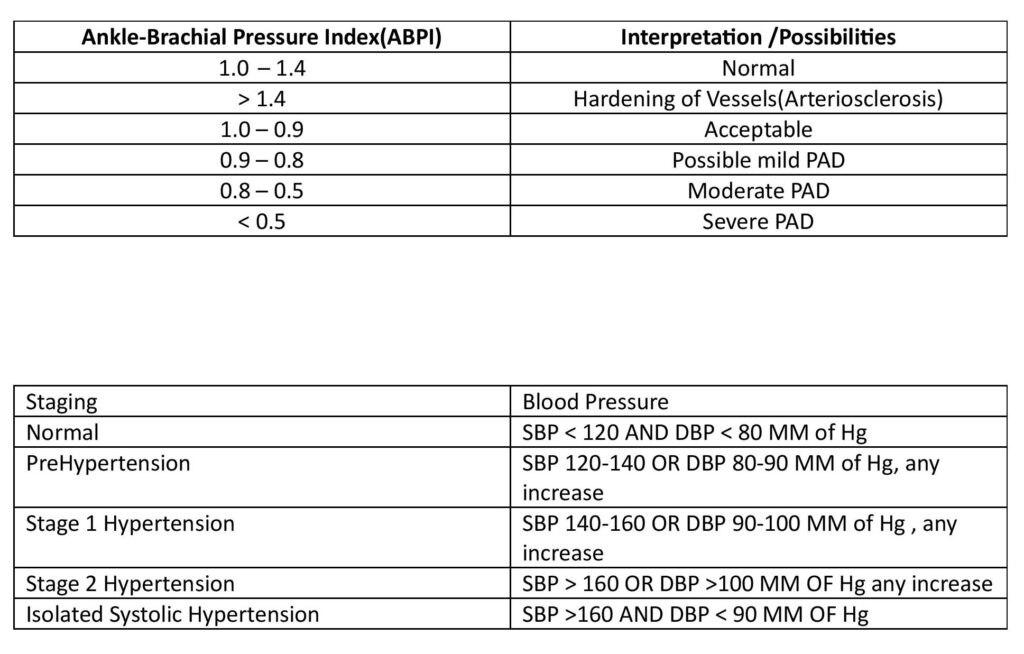
1. Cardiovascular Disease (CVD)
Screening:
Lipid profile (annual or more frequently if abnormal).
Resting ECG if symptomatic or at high risk.
Blood pressure at every visit.
Signs to Monitor:
Hypertension, dyslipidemia, or chest pain.
Management:
Statins, antiplatelets, or beta-blockers as indicated.
Lifestyle modifications (exercise, diet).
2. Peripheral Artery Disease (PAD)
Screening:
Ankle-brachial index (ABI) if symptomatic or high-risk.
Signs to Monitor:
Intermittent claudication or reduced pulses.
Management:
Smoking cessation, antiplatelet therapy, and revascularization if necessary.
3. Cerebrovascular Disease
Screening:
Monitor for stroke/TIA symptoms, especially in high-risk individuals.
Management:
Blood pressure and lipid control, anticoagulation if atrial fibrillation is present.
Other Areas
1. Oral and Dental Health
Regular dental check-ups for periodontal disease and infections.
2. Mental Health
Screening for depression or anxiety (common in diabetes).
3. Gastrointestinal Health
Monitor for gastroparesis, diarrhea, or constipation.
Routine Monitoring Checklist
Glycemic Control: HbA1c every 3–6 months.
Lipid Profile: At least annually.
Blood Pressure: At every visit.
Foot Examination: Annually or more frequently in high-risk patients.
Weight and BMI: Regularly.
Immunizations: Influenza, pneumococcal, and hepatitis B vaccines.
By systematically monitoring these areas, you can address complications early and improve the quality of life for people with diabetes.