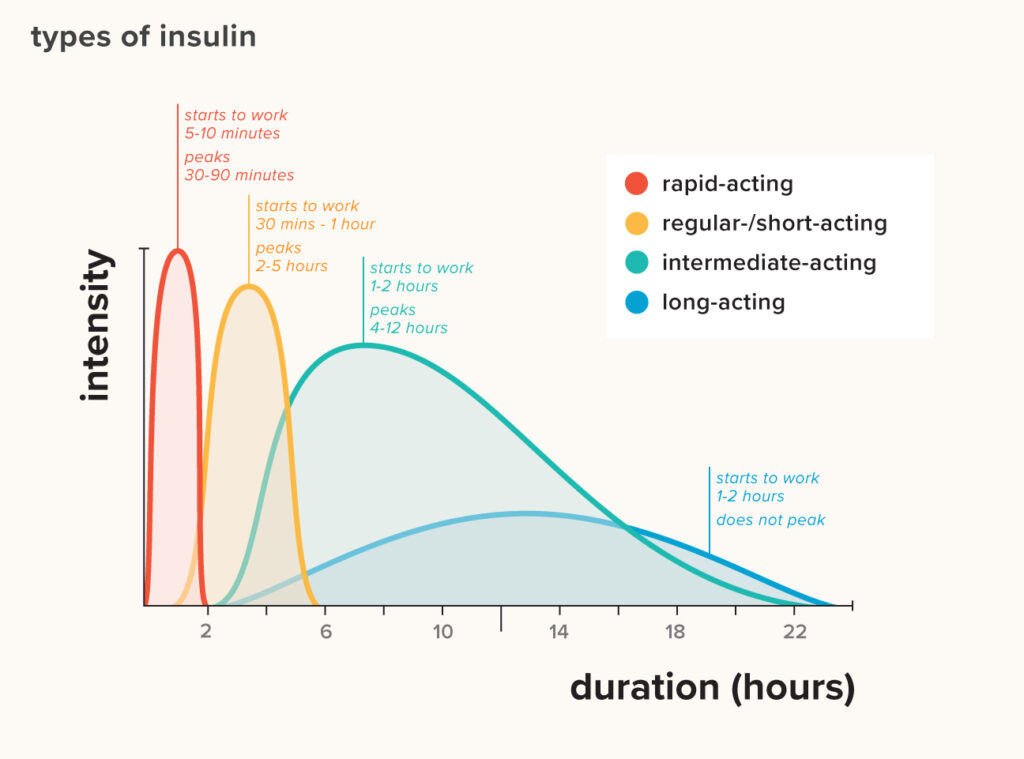
Intermediate-acting insulins are a type of insulin used to control blood sugar levels in people with diabetes, particularly in those who require a longer duration of action than short-acting insulins provide. These insulins typically start working within 1 to 3 hours after injection, reach their peak effect between 4 to 12 hours, and can last for up to 18 to 24 hours.
Examples of Intermediate-Acting Insulins:
- NPH (Neutral Protamine Hagedorn) Insulin:
- Also known as isophane insulin, NPH insulin is the most common intermediate-acting insulin.
- It appears cloudy and needs to be mixed before use.
- NPH insulin is often used in combination with short-acting or rapid-acting insulins to provide a more flexible insulin regimen that can cover both basal (background) and bolus (mealtime) needs.
- Premixed Insulins Containing NPH:
- These are pre-mixed formulations that combine intermediate-acting NPH insulin with a short-acting or rapid-acting insulin. Examples include Mixtard (a mix of soluble insulin and NPH insulin) and Humulin M3.
- These pre-mixed insulins simplify the injection regimen by combining both components into a single injection.
How Intermediate-Acting Insulins Are Used:
Intermediate-acting insulins are often injected once or twice daily, depending on the individual’s needs and their doctor’s recommendations. They are typically used to manage blood sugar levels between meals and overnight. Because of their longer duration of action, intermediate-acting insulins provide a steady, baseline level of insulin to help control blood sugar throughout the day and night.
Mixtard insulin is a type of pre-mixed insulin used to manage blood glucose levels in people with diabetes. It contains a combination of two types of insulin:
- Short-acting insulin (soluble insulin): This insulin works quickly to reduce blood sugar levels after meals.
- Intermediate-acting insulin (isophane insulin or NPH insulin): This insulin takes longer to start working but helps maintain lower blood sugar levels throughout the day and night.
The combination of these two types of insulin in Mixtard provides both immediate and longer-lasting control of blood sugar levels. It is typically injected subcutaneously (under the skin) and is used by people with diabetes who need a consistent insulin regimen that covers both mealtime and background insulin requirements.
Insulin therapy dosing varies greatly depending on the individual’s needs, type of diabetes, lifestyle, blood glucose levels, and other factors. Here are a few examples of insulin therapy dosing for different situations:
1. Basal-Bolus Insulin Regimen:
This regimen involves the use of long-acting (basal) insulin to provide a constant level of insulin throughout the day and night, along with short-acting or rapid-acting (bolus) insulin to control blood sugar spikes after meals.
- Basal Insulin Dose: Long-acting insulin (e.g., insulin glargine or insulin detemir) is usually administered once daily, at the same time each day. The typical starting dose might be 10 units or 0.2 units per kilogram of body weight, adjusted based on blood glucose levels.
- Bolus Insulin Dose: Rapid-acting insulin (e.g., insulin lispro, aspart, or glulisine) is administered before meals. The dose is typically calculated based on carbohydrate intake (using a carbohydrate-to-insulin ratio) and current blood glucose level (using a correction factor or insulin sensitivity factor). Example:
- A person might use 10 units of insulin glargine once daily for their basal insulin.
- They might also use 1 unit of insulin lispro for every 10 grams of carbohydrates consumed at each meal, plus additional insulin if their blood glucose is above target.
2. Premixed Insulin Regimen:
This regimen involves the use of premixed insulin, which combines intermediate-acting insulin with short-acting insulin in a fixed ratio. This is often used for people who want to minimize the number of injections per day.
- Premixed Insulin Dose: Premixed insulin (e.g., 70/30, which means 70% NPH insulin and 30% regular insulin) is usually administered twice daily, before breakfast and dinner. Example:
- A person might use 20 units of 70/30 premixed insulin before breakfast and 15 units before dinner.
3. Once-Daily Basal Insulin:
For some individuals with type 2 diabetes, using only a long-acting basal insulin might be sufficient, especially if their insulin requirements are lower and they are also taking oral medications.
- Basal Insulin Dose: A single dose of long-acting insulin (e.g., insulin glargine or detemir) is administered once daily, often starting with 10 units per day or 0.1-0.2 units per kilogram of body weight. Example:
- A person might start with 10 units of insulin glargine once daily, adjusting the dose based on fasting blood glucose levels.
Important Considerations:
- Personalization: Insulin dosing must be individualized based on a person’s blood glucose levels, lifestyle, eating habits, and sensitivity to insulin.
- Monitoring: Regular blood glucose monitoring is essential to adjust insulin doses and prevent hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar).
- Consultation with Healthcare Providers: Always consult a healthcare provider to determine the most appropriate insulin regimen and dose. They can provide guidance based on continuous glucose monitoring (CGM) or self-monitoring of blood glucose (SMBG) data.
These examples are general and should not be used as medical advice. The exact dose and regimen should always be tailored to the individual’s specific needs and determined by a healthcare professional.
The choice of an insulin regimen will ultimately depend on an individual’s lifestyle, ability to administer and cope with insulin therapy, and their likely compliance.
Two important factors that impact insulin dosage are the insulin-to-carbohydrate ratio and insulin sensitivity.
Insulin-to-carbohydrate ratio: This is the amount of carbohydrates (in grams) that will be neutralized by 1 unit of insulin. For example, if a meal has 30 grams of carbohydrates and it raises blood sugar by 75 mg/dL, and it requires about 3 units of insulin to bring it back to baseline, then 3 units of insulin were needed to neutralize 30 grams of carbohydrates, or 1 unit of insulin per 10 grams of carbohydrates. This is the insulin-to-carbohydrate ratio for this patient. This ratio may differ from patient to patient and can vary slightly depending on the time of the meal and the type of carbohydrate.
Insulin sensitivity: This refers to the amount of blood sugar lowered by 1 unit of insulin, in the absence of food. If we look at the insulin sliding scale, we assume this to be 1:25 mg/dL.
Let’s take an example:
- Insulin-to-carbohydrate ratio: 1:12 grams
- Insulin sensitivity: 1:25 mg/dL
- Premeal glucose: 190 mg/dL
- Target blood glucose: 140 mg/dL
- Estimated meal carbohydrates: 72 grams
Calculation:
- 72 grams / 12 = 6 units of insulin required to neutralize the meal’s carbohydrates.
- (190 – 140) / 25 = 2 units required to correct blood glucose to the target.
Total units required: 6 + 2 = 8 units.